As an Amazon Associate, Dressage Today may earn an affiliate commission when you buy through links on our site. Products links are selected by Dressage Today editors.
You might have noticed that you’ve been hearing the phrase “hindgut health” in conversations about horses more so now than ever before. What does “hindgut health” mean in the context of your horse and what does it mean for you as his owner?
In this article, we break down the basics with help from experts Frank Andrews, DVM, LVMA equine committee professor and director of the Equine Health Studies Program at Louisiana State University in Baton Rouge, Louisiana, and Christina (“Cricket”) Russillo, DVM, a senior associate at Virginia Equine Imaging in The Plains, Virginia. Remember, in addition to the information provided in this article, always be sure to consult your veterinarian about what is best for your horse as an individual.
Hindgut Basics
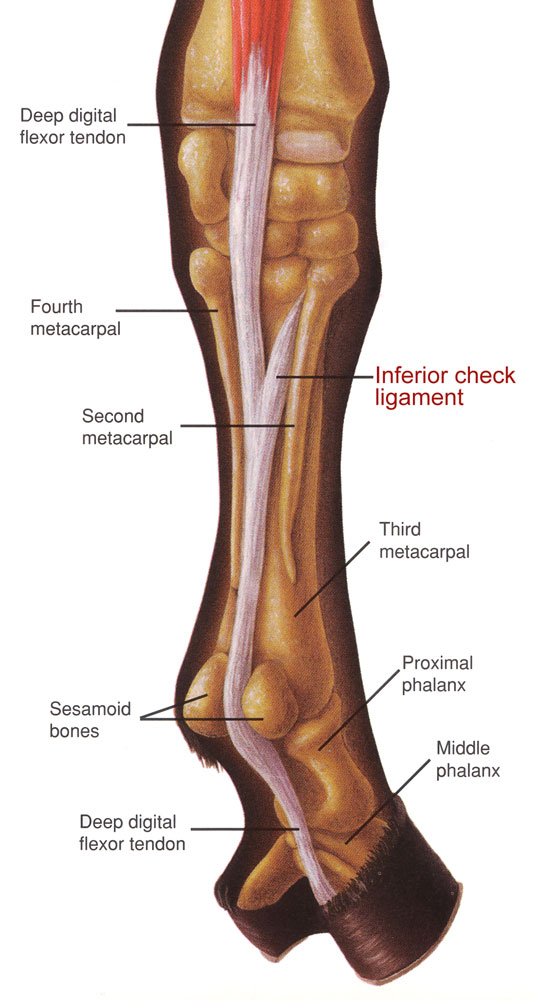
The horse’s hindgut—or large intestine, which includes the cecum and colon—is essential to the function of the horse’s overall digestive system and is important for bacterial content. When feed is processed in the horse’s digestive system, it is fermented and digested by bacteria in the hindgut. Fermentation is the chemical breakdown of substances by bacteria, yeast or other microorganisms.
Fermentation provides the horse with energy, vitamins, minerals and amino acids. When the horse suffers from poor hindgut health, he lacks these key dietary components. A lack of proper fermentation not only results in a decrease of these dietary essentials, but also in poor feed utilization, poor appetite, dehydration, poor coat and hoof condition, reduced immune function and a change in attitude. These negative effects will ultimately result in poor performance and training.
Horses are biologically designed to continuously consume small amounts of food, such as pasture grass throughout the day. However, the modern performance horse often has a lifestyle that vastly differs from this model of continuous grazing. When inherent habits like this are disrupted, compromised or totally eliminated and improperly substituted, then the horse is immediately at risk for digestive issues, Andrews says.
Problems in the Hindgut
Horses can experience a wide variety of hindgut health issues, ranging from diarrhea to torsion colics. However, according to Russillo, the most commonly occurring hindgut health issue in the performance horse is colonic ulcers, which are the focus of this article.
“Colonic ulcers are the number-one thing I deal with in my patient population,” she says. “Other issues that can pop up include infectious causes of diarrhea [such as Potomac horse fever], large bacterial shifts in the colon caused by orally administered antibiotics and dietary intolerances [for example, caused by changes in pasture]. But by and large, the thing that we’re day in, day out screening for in the performance horse is definitely going to be ‘could this horse have colonic ulcers?’” Russillo says.
What is a Hindgut Ulcer?
An ulcer can be defined as a thinning of the lining of the gastrointestinal tract. Ulcers can occur in the foregut (stomach) and are also referred to as gastric ulcers. However, ulcers can also occur in the hindgut, specifically in the colon, and are therefore referred to as colonic ulcers.
Andrews defines a hindgut ulcer as a depression of the lining of the colon. Hindgut ulcers are difficult to diagnose and often require an ultrasound. The severity of the condition is determined by the thickness of the colon’s outer wall.
Colonic ulcers are extremely difficult to truly diagnose because it is impossible to thoroughly examine the colon without surgery. “Surgical diagnosis of colon ulcers is the true gold standard, because the surgeon can either visualize the ulcer or perform a biopsy that can be examined microscopically to determine the degree of ulceration,” Russillo says. While surgery isn’t typically recommended to diagnose ulcers, it’s more indicative of just how hard it is to really understand to what degree a horse is affected, she explains. “Hence, we utilize the combination of clinical signs, ultrasound and blood work.”
Gastric ulcers have been a popular topic of discussion for years, but the conversation about colonic ulcers, on the other hand, has recently increased. Russillo attributes this to a greater awareness that the problem exists in the first place. “Awareness and education are primarily why there’s been an increase in this discussion. We just now know that we need to look for it,” she says.
How Common Are Colonic Ulcers?
Ulcers are a common issue in performance horses. Russillo references a study performed in 2005 by Franklin L. Pellegrini, DVM, that examined the presence of colonic ulcers in horses at necropsy. What could be concluded, based on the study, according to Russillo, is that somewhere between 44 and 60 percent of horses have some level of colonic ulceration, with a higher percentage in performance horses. “Stomach ulcers are still more prevalent,” she says. “But hindgut ulcers are definitely a real thing and worth having conversations with owners about.”
Clinical Signs
Hindgut ulcers tend to have more profound clinical signs than gastric ulcers, according to Andrews. Signs include a recurring lack of appetite, lethargy, intermittent fever, colic bouts, occasional edema on the belly from a loss of protein in the blood, weight loss and thin body condition. According to Russillo, typical signs include a combination of loose manure and large fecal balls or, in some cases, complete diarrhea. Liquid manure down the horse’s inner thighs and legs also serves as an indication.

When Andrews observes a horse with chronic issues of colic, diarrhea, lethargy or poor performance, he says people tend to think the horse is suffering from gastric ulcers. This is a common misconception. Typically, he says, these clinical signs actually relate to issues in the hindgut, which cannot be seen with an endoscope, so ultrasound examination and blood work are much more helpful. It should be noted that horses with colonic ulcers might have gastric ulcers as well due to stress, says Andrews.
Diagnosis
In order to diagnose colonic ulcers, veterinarians most often perform a transabdominal ultrasound. This involves an ultrasound examination of the abdomen, with a focus on the horse’s right side in an effort to visualize the right dorsal colon. This, according to Russillo, requires specialized equipment and skill on the part of the veterinarian in knowing where to look. Typically, the ultrasound is positioned between the horse’s ribs and directed toward the colon. The veterinarian then attempts to measure the colon’s outer layer, or serosa. However, given the complexity in diagnosing colonic ulcers, even if the findings indicate colonic edema, clinical signs must be incorporated into the diagnosis as well, Russillo says.

Clues from Blood Work
Hindgut ulcers can also be detected through blood work, which provides information, in this case, on the horse’s protein levels. First, they will observe a complete blood count, looking for low protein concentrations in the blood. However, the total protein is typically within normal limits, so a specific albumin test should be done.
Typically, if a horse is suffering from hindgut ulcers, his albumin (the primary protein) concentration is low. Also, if there is inflammation in the hindgut, there will be a spike in the horse’s globulin concentration.
Veterinarians also observe a horse’s hemogram, a test measuring both white and red blood cell counts. A hemogram detects anemia and infection. Horses with colonic ulcers will be mildly anemic, which means they have a deficiency in red blood cells, or hemoglobin, in the blood and will have a high white blood cell count, which denotes infection.
According to Andrews, veterinarians are now utilizing a test that detects serum amyloid A (SAA) proteins. This test determines if the horse is suffering from inflammation. Andrews explained that hindgut ulcers or any ulcerative condition is associated with inflammation and the release of acute-phase inflammatory proteins like SAA, which the test is used to detect. A high value could indicate hindgut ulcers and follow-up testing may show if treatment is effective, which would be indicated by a decrease in the SAA value. The caveat to this kind of test is that an increase in SAA is nonspecific and any inflammation in the horse’s body can lead to an increase in SAA, meaning it is not a test that can differentiate stomach ulcers from hindgut ulcers on its own.
Treatment and Preventive Measures
In terms of treatment measures for the hindgut, Andrews starts by reducing the amount of bulk in the horse’s diet. He says hay is considered a “high-bulk diet,” as it takes up a lot of volume in the large colon, requiring the colon to work harder to mix it and digest it. It is also scratchy. Instead, Andrews recommends pelleted feeds because the volume of materials in the hindgut is much smaller and less scratchy. These products digest quicker and the residual content is therefore smaller.
The colon’s job is to pull liquid from the horse’s food and absorb the nutrients back into his system and then package the waste into manure. If a horse is diagnosed with colonic ulcers, then it is vital for the colon to be given time to rest. To do this, owners must reduce the horse’s intake of long-stem fiber, which means eliminating hay intake. Hay is a lot of work for the colon to digest and process and, in this case, it can scratch and cause irritation to the hindgut. Instead, hay should be substituted with soaked alfalfa cubes, alfalfa pellets, beet pulp or a complete feed that includes a horse’s necessary daily dose of fiber.
Decreasing a horse’s hay may cause concern for some owners, as hay is commonly fed to horses. However, Andrews explains that this diet change is temporary. Any change in diet has the potential to cause colic, but in hindgut ulcers, this change is designed to decrease colic, one of the clinical signs associated with the condition. Therefore, by reducing the bulk in the diet, the colic episodes should actually resolve. However, if colic signs continue, then having the horse evaluated by a veterinarian is indicated and it might be that the dietary change needs to be more gradual and hay could be added back to the diet.
Andrews suggests the complete pellet diet for three months in order to treat colonic ulcers. Two complete pellet grains include an equine-senior and equine-adult grain, which are alfalfa hay based. Essentially, a complete pellet is grain and forage wrapped in one feed source. It is designed to totally replace hay and forage in the horse’s diet and label directions should be followed carefully so that the horse is fed the right amount.
Andrews also tends to prescribe corn oil or flaxseed oil. This coats the intestine and supplies omega fatty acids, which are anti-inflammatories for the large intestine. Typically, he suggests one cup of corn oil two times a day mixed with the senior or equine adult feed. The oil, he says, must be slowly introduced. If the horse is given too much at once, there is a chance the horse will refuse his grain.
Andrews also suggests twice-daily doses of psyllium, which is similar to Metamucil for humans. This component coats the intestine and has anti-inflammatory properties. He mentions other products that contain psyllium along with prebiotics and probiotics. It also acts as a laxative; Andrews has found that this laxative tends to lubricate the hindgut and help move feed through the colon and helps the digestive system heal.
In addition to nutritional components and changes, Andrews suggests that owners take their horses off any and all nonsteroidal anti-inflammatories (NSAIDs), such as phenylbutazone (bute) and Banamine. He recognizes that, in some cases, older horses who suffer from chronic arthritis may need these medications on a prescribed maintenance dose. His warning, however, is that these medications tend to exacerbate hindgut ulcers or may even cause the condition in the first place.

After removing these medications, he typically prescribes sucralfate. This is a pharmaceutical coating agent, approved for treating ulcers in humans. This product is not approved for horses, so he uses the human formula when administering. He advises owners to avoid compounded products, which he admits, is hard to do. This is because compounded products are not approved by the U.S. Food and Drug Administration (FDA) and the drug concentration of the compound is not verified or checked. Andrews typically uses human drugs (when an FDA-approved product is not available for horses) to treat horses with this condition because these medications are required to undergo a very rigorous FDA approval process.
Essentially, Russillo says that prevention comes down to attempting to understand potential triggers and managing the horse’s lifestyle. In the case of the performance horse, these animals tend to live a very fast-paced, high-stress lifestyle. Although we can’t always eliminate stressors, we can try to balance them as best we can. It is the owner’s responsibility to manage stress levels and provide the best maintenance routine and, when needed, the best treatment and preventive measures.
An Introduction to Gastric Ulcers
Although gastric ulcers and colonic ulcers are similar in the sense that they are both a thinning of the lining of the gastrointestinal tract, they are very different. They occur in different parts of the horse’s digestive tract, present differently, are diagnosed differently and in some instances, require almost opposite treatments.
Gastric ulcers, or stomach ulcers, occur in the horse’s foregut and are a result of a break or erosion in the lining of the esophagus, stomach or small intestine. Cricket Russillo, DVM, a senior associate at Virginia Equine Imaging in The Plains, Virginia, explains that stomach ulcers typically occur in either the nonglandular region, the upper portion of the stomach, or the glandular region—the lower portion of the stomach.
Clinical Signs and Diagnosis
Clinical signs of gastric ulcers can include changes in attitude, poor appetite, colic, decreased performance, decline in body condition, weight loss and lack of energy.
To diagnose stomach ulcers, veterinarians use an endoscope. In order to perform the procedure, referred to as a gastroscopy, the horse must have fasted for 12 hours, with an exception given to water. Using a fiberoptic camera, the veterinarian inserts the endoscope through the horse’s nostril, into the back of the throat, until the horse swallows it. Then the camera is directed down the esophagus until it reaches the stomach.
According to Russillo, it is vital that all areas of the stomach be looked at for any indication of ulcers, inflammation or other irritation. A complete evaluation is crucial since horses can have ulcers in multiple areas of the stomach.
In the case of a stomach ulcer, there is a grading scale from 0 to 4; 0 indicates a healthy, non-irritated stomach, whereas 4 indicates the stomach is suffering from severe ulcers and ulcerations. The maximum grade essentially, indicates a complete loss of the epithelium. Grade 4 ulcers are large, coalescing and full thickness (with complete loss of the epithelial lining of the stomach), often with associated hemorrhage. This is called Equine Gastric Ulcer Syndrome (EGUS).
Treatment and Prevention
Russillo suggests feeding a low-starch/low-sugar diet; as in excess, it causes more acid in the horse’s digestive system. Opposite from colonic ulcers, stomach ulcers, in order to heal, require that the horse be eating and digesting at all times. This means having free-choice access to pasture and hay. A popular product, the NibbleNet, a slow-feeder hay net, has been found quite effective in these cases, as it prevents the horse from getting fat but still encourages him to continuously eat. Russillo also encourages multiple grain meals throughout the day, as opposed to the conventional morning and evening feedings.
She also encourages owners to make environmental changes for their horses. This means providing as much free pasture time as possible. She explains that horses are naturally designed to eat and graze all throughout the day and because of their natural bodily function and design, they need to have something in their system to buffer their constant acid production.
According to Russillo, there is current thinking that suggests that gastric ulcers that occur in the pyloric region of the stomach may respond better to misoprostol and sucralfate, but the ulcers in the squamous portion of the stomach seem to still respond well to omeprazole. Omeprazole is a medication that inhibits the proton pump in a horse’s stomach.
Russillo says that when owners utilize omeprazole-based products, they always need to ask for FDA-approved medication. There are a myriad of omeprazole-based products on the market that claim to cure gastric ulcers. However, the FDA has issued warnings that these products are unsafe and ineffective, as they contain varying levels of omeprazole, some at sub- or excess therapeutic levels. As of now, there is only one product officially approved to cure and prevent gastric ulcers. If clinical signs haven’t resolved after diet and medications have been appropriately adjusted, owners should also consider adjusting the horse’s training program.
According to Russillo, in the case of a performance horse, although it may not be practical, removing a horse completely from his training program may be necessary in order to give the body time to rest and heal.
Christina “Cricket” Russillo, DVM, graduated from the Tufts University School of Veterinary Medicine in 2001. Following graduation, she completed a large animal medicine and surgery internship at Texas A&M and realized her desire was to work on elite sport horses. After 13 years of practice at Fairfield Equine Associates in Newtown, Connecticut, focusing on high-level show-jumping and dressage horses, she joined Virginia Equine Imaging in June 2015. Russillo relocates to Florida every winter to support her clients and patients in Wellington and the surrounding areas. She is a member of the International Society for Equine Locomotor Pathology and hopes to attain certification next year. In February 2017, Russillo was appointed the U.S. Dressage Team veterinarian. In addition to her busy schedule focused on sports medicine, she enjoys spending time outdoors with her husband and daughter. She has competed through Third Level and loves to play tennis.
Frank M. Andrews, DVM, MS, is a graduate of Washington State University College of Veterinary Medicine in Pullman, Washington, where he received a DVM and MS. He completed an equine internal medicine residency at The Ohio State University in Columbus, Ohio. After 20 years at the University of Tennessee College of Veterinary Medicine, he is currently LVMA Equine Committee Professor and Director of the Equine Health Studies Program at Louisiana State University School of Veterinary Medicine. Andrews is Diplomate in the American College of Veterinary Medicine (ACVIM). He was staff equestrian veterinarian for the 1996 Summer Olympics in Atlanta, Georgia, and has clinical and research interests in digestive health and nutritional and pharmacologic management of stomach and colonic ulcers in horses.