You stuck it out through the winter, diligently driving to the barn through snow and ice so that you wouldn’t lose time during your spring training. As the ground starts to thaw and temperatures rise, you are thrilled to find that your horse is progressing well. Your trainer says that he’s looking better than ever and you should be ready to move up soon. But just as you’re starting to dust off your show coat and plan your summer competition schedule, you notice that your horse’s breathing looks a little more labored and his skin starts to show signs of irritation. You carefully observe your horse over the next few days and find that his symptoms are worsening. Your otherwise healthy horse appears to be struggling to stay comfortable. What could be to blame?
Seasonal equine allergies might be the culprit. Much like humans, horses’ bodies respond to allergens, triggering a chain of reactions. Generally speaking, an allergy is a hypersensitivity reaction that occurs when a horse or a person’s immune system reacts excessively to any kind of foreign substance or antigen, also known as an allergen. See The Comprehensive Guide to Equine Veterinary Medicine by Barb Crabbe, DVM.
Horses can display allergies to a variety of stimuli, ranging from vaccinations to certain ingredients in feed to mold spores in the air or even something such as a bug or plant to which their skin might be exposed. Allergic reactions are alarming for several reasons. One is that they often affect important systems in the body, such as the lungs or skin. Allergies affecting these areas can often cause inflammation, or mucous production in the airways or fluid swelling of the skin that results in itching or hives.
Identifying, diagnosing and effectively treating seasonal equine allergies can be exceptionally challenging. The sheer number of variables in a single horse’s environment—ranging from shavings and dust to pollen and molds to feeds and fly sprays—makes it is nearly impossible to isolate the particular cause of a reaction. If you suspect that your horse is suffering from an allergy-related cause, be sure to consult your veterinarian so that your horse can be evaluated on an individual basis.
In order to help you make the most educated decisions possible regarding your horse’s health, we have compiled a list of some of the lesser-known facts about seasonal equine allergies with explanations from top professionals in the field. John Madigan, BS, DVM, MS, professor of equine medicine in the department of medicine and epidemiology at the University of California, Davis, School of Veterinary Medicine, and Kathy Williamson, DVM, manager of veterinary services at Purina Animal Nutrition, answer some of the more mystifying questions regarding equine allergy problems.
How prevalent are seasonal equine allergies?
Madigan estimates that only about 10 percent of the equine population suffers from allergies.
What are the most common allergies horses deal with?
Of the fraction of the population that does experience difficulty with seasonal allergies, Williamson says that insect-bite hypersensitivity—especially from culicoides or biting midges—is the most common seasonal allergy she has observed among mature and otherwise healthy working horses.
According to Williamson, tree and plant pollens—such as cedar—and topically applied fly repellents also rank high on the list of common allergy sources.
Madigan explains that in his experience, heaves or recurrent airway obstruction (RAO), caused by a hypersensitivity to molds in hay is common. This typically results in difficulty breathing, coughing or wheezy lungs. “Dermatologic reactions with hives, where horses are reacting to something in their environment, can also create this same kind of mystery,” he says.
Reactions to vaccinations and to feeds can also fall into the category of allergic reactions or hypersensitivities but they don’t often have a seasonal component.
What are typical symptoms of allergic reactions?
Allergies in horses most commonly manifest in skin abnormalities, ranging from hives to areas of hair loss, known as atopic dermatitis or atopic skin disease, Williamson says. This may appear only in distinct areas or the whole body may be affected. “Most often the horse will suffer from intense itching. The skin abnormality may wax and wane, especially if the allergen is seasonal. Additionally, one of the earliest signs of allergic airway disease in horses may be exercise intolerance. Other signs may include coughing and increased effort on expiration of breath,” she says.
Is geographic location a factor?
“Unfortunately, there are potential allergens everywhere,” says Williamson as she explains that each geographical area has its own group of possible allergens. This is because plant, tree and insect populations vary with geography. “Specifically, while practicing in Maryland and Oklahoma I treated many horses for presumed hypersensitivity to cedar tree pollen and sap,” she says.
How long does it take an allergy to develop?
Horses can develop an allergy upon first exposure to a substance, Madigan says. “You can have a hypersensitivity to something the first time you see it. On the other hand, it might take weeks, months or even years for an allergy to emerge. A 20-year-old horse with no history of allergies can one day appear to have an allergic reaction.”
Are there factors that can predispose a horse to allergies?
The jury is still out on whether horses can be predisposed to an allergy condition. Some sources report that age, breed or gender have no affect on susceptibility to allergy conditions. Madigan explains that there might be certain bloodlines within horses that tend to experience more allergy issues, but as a whole, he has not observed any other factors that might predispose a horse.
Williamson says that in her experience, she has seen that allergy cases tend to noticeably crop up in Arabians and Thoroughbreds. Outside of bloodlines and breeding, she says that non-allergic skin conditions might predispose a horse to further problems, or dietary conditions in which a horse’s diet lacks proper fatty acids for skin and hair-coat health. “Round- bale feeding and stall confinement are also considered significant risk factors in the development of RAO,” she says.
How do allergies affect a horse’s ability to work?
According to Madigan, allergies can be incapacitating with regard to performance. “You’d have to get an evaluation of the magnitude of the problem,” he says. “If your vet hears a lot of wheezing, that will certainly limit what you can do. The horse might be able to go for a walk, but when you need oxygen, which is necessary for work and performance, and you’re facing issues of bronchoconstriction, that can be a problem. They have inhalers that they treat horses with just for that reason. It can be part of a risk factor in their work,” he says.
What is considered prime allergy season?
The warmer months can typically present the most trouble for horses with allergies because many of the typical allergens, such as bugs and mold, thrive in hotter weather. Madigan explains that one of the biggest and most troubling seasonal allergic disorders is a hypersensitivity to the biting midge. The horse’s reaction to midge bites is also commonly known as sweet itch. These insects feed on the abdomen or the tail head or up by the mane. “These little gnats release something that horses can be extremely hypersensitive to. These bugs hatch from water so that when the weather warms up, they emerge, and that’s a big factor,” he says.
Why are allergies challenging to diagnose?
According to Madigan, it is challenging to diagnose an allergy because horses can suffer from viral, bacterial, fungal and hypersensitivity/allergy problems and it is easy to mislabel a certain issue. Within hypersensitivity issues alone, a reaction could be caused by feed, an aerosol or something topical.
“You’ve got to be lucky to figure out a particular trigger,” he says, “because, how many things could it be? Just go ahead and think about possible causes. There are a lot. It could be shavings, it could be dust, it could be pollen…. It is a nightmare.”
What kinds of treatment options are available?
“The way to narrow down the possibilities of allergens on that long list of variables is by beginning with symptomatic treatment and then maybe to start making some changes,” Madigan says. “Or you hope that it goes away after symptomatic treatment. If it doesn’t, then you can start with the testing.”
If possible, it is best to eliminate the cause or avoid contact with a particular allergen. If that isn’t possible, symptomatic treatment options include the use of antihistamines and corticosteroids.
There are also several different allergy tests available, such as blood (serum) or skin testing. One particular kind of testing, known as the radioallergosorbent test (RAST), involves a blood sample taken to study the amount of allergen-specific antibodies that are present. When the body encounters something that it is allergic to, it produces antibodies against it. These antibodies then signal the body to release certain chemicals, such as immunoglobin E, or IgE, which is strongly linked to the body’s allergy responses. The RAST identifies allergy triggers by looking for these allergen-specific antibodies.
While this kind of testing can be helpful in some cases, Williamson says that the veracity and accuracy of various (blood) serum allergy-testing methods in horses have been studied and reported in the scientific literature by numerous researchers during the last 15 years and they don’t always provide answers. “The results of the research do not support the use of current serum allergy-testing methods to identify specific allergens associated with allergic diseases in horses,” she says.
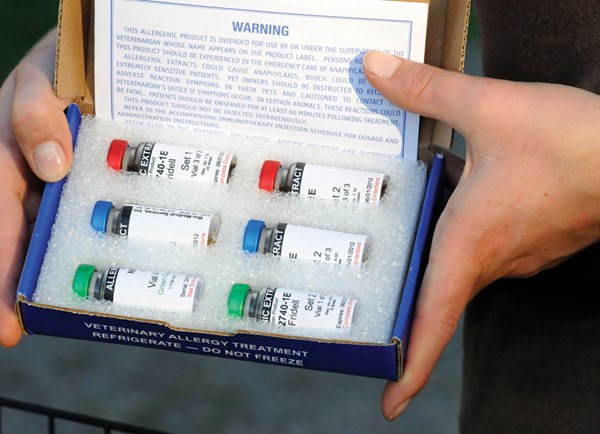
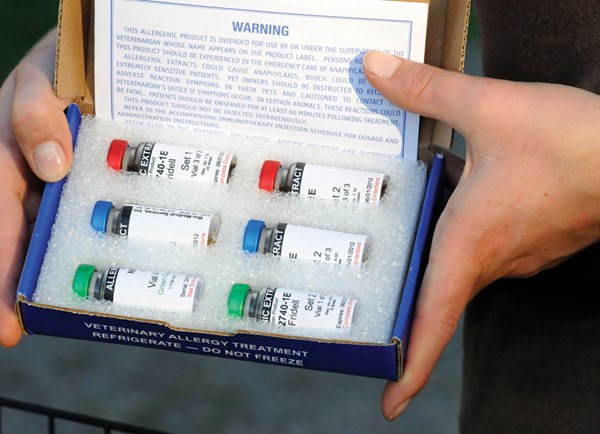
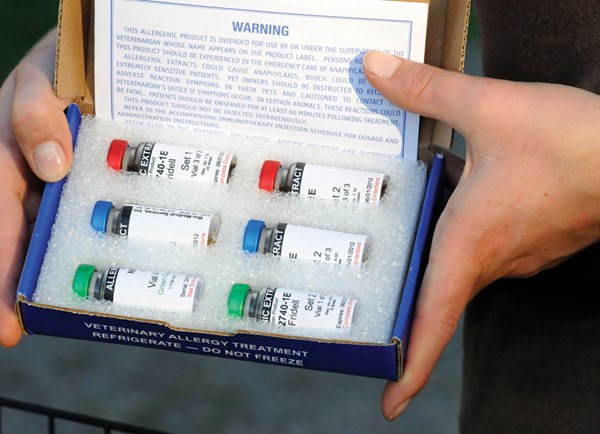
With skin testing, a vet will make a pattern on the horse’s skin in which 15 to 20 various allergens that the horse could be exposed to are injected. “This allows you to see if they develop a hive or an immediate hypersensitivity reaction. That kind of skin testing is equivalent to the scratch testing in people,” Madigan says. Based on results of the tests, it is possible to then administer allergy shots to overwhelm the immune system, thereby down-regulating the body’s response.
Can new technology help?
Unfortunately, the work to improve diagnostic and treatment options for allergies in horses is ongoing, Williamson says. “Horses present a significant challenge for specific allergen identification due to the fact that they have such high levels of circulating IgE—the antibody associated with the allergic response,” she says. Additionally, it is now believed that other immunoglobin subtypes may play a role in equine allergies, which can complicate testing that identifies allergen-specific IgE, such as blood-serum allergy testing.
“Recent studies of allergen-specific immunotherapy in horses have shown promise particularly with regard to atopic skin disease. However, similar studies in horses with insect-bite hypersensitivity did not show promising results,” she explains. Even more problematic is the fact that certain medications often prescribed by veterinarians to help control allergies are no longer available or are very difficult to procure currently, according to Williamson.
Although new supplements and products abound on the market, she says that she is not aware of any products that are backed by robust scientific studies that demonstrate efficacy.
What options do horse owners have to manage allergies?
The variable nature of allergic diseases in horses requires that each case be handled individually with regard to prevention, diagnosis and treatment. Williamson recommends consulting closely with your veterinarian, who will be familiar with the common allergens and allergic diseases affecting horses in your area, to determine the best options for your situation.
Is Headshaking Allergy Related?
Headshaking is a condition in which a horse shakes, flicks or jerks his head uncontrollably without any obvious cause. This response can occur constantly, intermittently or even seasonally. Each individual case can be caused by a variety of different stimuli, but the body’s response to the stimuli tends to be the same throughout all horses with some variation in severity.
John Madigan, BS, DVM, MS, and a team of researchers have performed extensive study in the field of equine headshaking and have determined that rather than being allergy related, it is caused by an abnormal function of the trigeminal nerve. This causes severe neuropathic pain over the area of the face. Out of the horses that are headshakers, some are called “photic headshakers,” meaning that their symptoms are brought on by exposure to bright light. Exercise can also trigger headshaking in horses, but it is possible that this occurs because changes that arise in a horse’s body when he exercises, such as changes in heart rate or sweating, could cause the nerve system to misfire.
So why is headshaking not considered an allergic response? “That’s a good question and it comes up pretty frequently because there is a very seasonal component and there are a variety of triggers to headshaking,” Madigan says.
Springtime onset is fairly common, according to Madigan. This seasonal onset can be misleading because although headshaking might become more common during allergy season, that doesn’t mean that it necessarily stems from allergy problems. It is more likely that the body is responding to the changes in sunlight in an attempt to acclimate to longer days and warmer temperatures.
It is possible that many horse owners often misattribute headshaking to allergies because the clinical signs, such as an itchy and runny nose, are similar to what people experience when they have allergies. The difference, Madigan points out, is that headshaking comes from neuropathic pain, which causes a burning, tingling, itching or electric-like sensation, and is mediated by the trigeminal nerve. Many allergies can be resolved with help from antihistamines or corticosteroids, and headshakers don’t typically respond to these medications.
“Headshaking is a very difficult disorder to study because neuropathic pain can be intermittent and seasonal,” Madigan says. Sometimes, a horse owner can make a change in the horse’s management and he will stop headshaking. But it is possible that the horse stopped headshaking because he reached the end of his headshaking cycle, not because the change in management resolved the problem. When a horse stops headshaking, sometimes the owner makes the mistake of assuming that the last change made in the horse’s management was the key. But then around the same season the following year, the headshaking returns. To assess whether an improvement in treatment actually occurred, Madigan recommends studying the horse for a full year of evidence that the horse has improved due to the intermittent seasonality of headshaking.
For more information about this disorder, visit headshakerinfo.org.
John Madigan, BS, DVM, MS, is a professor of equine medicine in the department of medicine and epidemiology, at the School of Veterinary Medicine, University of California, Davis. He earned his DVM degree at UC Davis in 1975 and is a diplomate of the American College of Veterinary Internal Medicine. Madigan is also internationally recognized for his contributions to equine medicine, neonatal care and animal welfare and rescue. His study of equine clinical neurology is focused on equine headshaking syndrome.
Kathy Williamson, DVM, is the manager of veterinary services at Purina Animal Nutrition. She supports all veterinary functions on the Purina Farm and is the key advisor to the horse group on veterinary relations and medical issues. Williamson received her degree in veterinary medicine from Iowa State University and has a background in equine practice and racetrack regulatory medicine. She has competed in dressage and combined training for more than 30 years.