As a dressage rider with riding pain, my story is not an uncommon one. After spending over 40 years of my life as a dressage rider, teaching and training, I was not able to get on a horse without extreme riding pain. Along the way, I learned firsthand that dressage riders can be more susceptible to developing problematic hip joints due to the motions they make to follow the dressage horse’s movement. Four years, 19 doctors and other health practitioners, two arthroscopic hip surgeries and $25,000 later, I finally got properly diagnosed and treated for femoroacetabular impingement syndrome (FAIS) in my hip to, at last, get back in the saddle. I hope this article helps others who might be in similar situations of riding pain and hip surgery.
Diagnosing My Riding Pain
It all began in 2007, when a standard dismount caused me to buckle from pain upon landing on my right leg. It had simply given out as soon as it touched the ground, and I grabbed the saddle so as not to fall. ?It had been an uneventful ride, except for a small sideways spook that had left me standing in my right stirrup while my horse moved abruptly to the left. During the spook, I felt a twinge in my right hip and lower back area but believed it insignificant. That is, until I dismounted. ?I managed to walk far enough to put my horse away before calling the doctor.
His diagnosis was a severe groin pull or labral tear (the labrum is a type of cartilage that lines the hip socket). One required rest, the other surgery. He felt unqualified to make the diagnosis of labral tear and referred me to a specialist. I knew my health-insurance options were limited because of the high deductible plans that are one of the challenges of being self-employed, so I chose the conservative option of rest.
I supplemented my treatment with the Rolf Method of Structural Integration (RSI) that I have used successfully for many years for other problems. It works to straighten misaligned body parts that have been damaged or shifted through accidents or surgeries. It also works to change patterns that have developed through repetitive movements that can create imbalances in the body over time. Just as a wheel that
is misaligned on your car can create all sorts of compensatory problems in your vehicle, misalignment of body parts that have been injured or overused can create compensations that ripple through your whole body and leave detrimental effects as we age. (To learn more about RSI, go to gravityheals.com.)
Between the anti-inflammatories and some RSI sessions, my hip pain initially decreased enough for me to ride. However, there was still an underlying discomfort that was getting progressively worse. I began to suspect the problem was very complicated, but it would take me another year, two more doctors and more X-rays and MRIs with contrast for an official diagnosis: femoracetabular impingement syndrome.
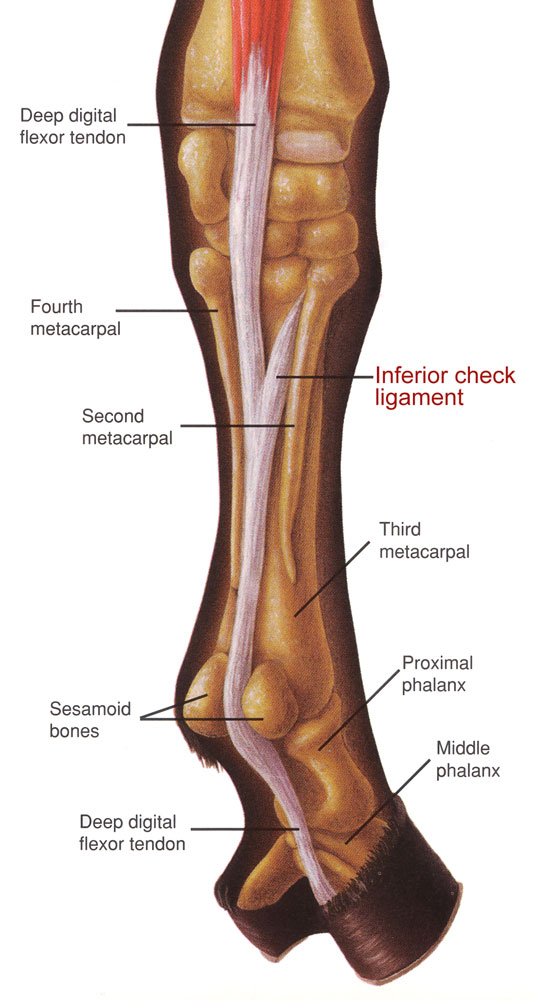
The medical policy of Anthem Blue Cross Blue Shield calls FAIS “an anatomical abnormality of the hip in which there is abnormal contact between the acetabular rim of the pelvis and the femoral head at the extremes of joint flexibility. Over
time, this contact may result in damage to joint cartilage, possibly leading to degenerative joint disease. Surgical treatment for this condition has been described and may involve either an open dislocation approach, arthroscopic surgery, or a combination of the two.”
In my case, the rim was not smooth because extra bone protruded into the joint, making the socket rough and compromising it. In addition, the ball had bony abnormalities that also contributed to the narrowing of the space between it and the socket. During certain motions of my leg, I would feel pain because those bony protrusions on the ball and socket would collide, causing a pinching motion. The lining and cartilage can also be damaged as a result of that pinch, which includes more permanent tears.
Of course, as I searched for answers and treatment options, I wanted to know why this had occurred. Fortunately for me, my physical therapist, Ann Herbert, is a rider and had suspected that I had FAIS well before any doctor did. She helped me understand that many activities that require repeated hip flexion and compression, such as riding, can cause underlying bony abnormalities to worsen. More research is needed to know if these activities create the problem or if most problems in the hip are a result of underlying defects exacerbated by particular occupations or pastimes.
Medicine has come up with several?options for people who have pain but do not have enough deterioration to merit joint replacement. Joint-preservation surgery is used when FAIS is present and there is still good joint space (when cartilage wears away, joint space diminishes to the point where bone touches bone). One type is open dislocation surgery, which provides full access to the joint and has been the gold standard until recently. Advancements in arthroscopic instruments and techniques have made it possible in some cases to use the arthroscopic approach instead. Avoiding or delaying a full or partial hip replacement is the primary goal of joint preservation surgery.
Hip Surgeries
My research and multiple consultations led me to? choose an arthroscopic repair called a “hip scope.” Due to insurance issues, I chose a local doctor? with a good reputation. It took about an hour, and I left the same day. After three weeks on crutches, followed by six weeks without riding or barn chores, I was allowed three more months of light work in each area. Rehab took its physical, mental and emotional toll. I had extensive physical therapy (paid out of pocket) and some RSI sessions. After six months, I could say that I had some relief but not as much as I had hoped or expected. I was able to ride, but still had some pain when I moved my leg into certain positions.
I had resigned myself to the fact that my only other option was a hip replacement when I took an unexpected fall while walking in the barn aisleway. The pain on the operated side was greater than before surgery but it also involved the right side of my lower back much more severely this time, near my sacro-iliac joint (SI).
During this stage of my medical adventure I learned that, over time, when there are problems in a hip joint, it stiffens to protect itself. Then, when a greater range of motion is needed, the SI tries to move instead. The vertebrae in the lower lumbar spine can be affected by hip joints that work unevenly also. The X-rays and MRI of my spine had been mostly negative, and no one seemed to think my lower back was the root of the problem. Still, I continued to have pain in that area.
It was suggested that I was experiencing referred pain (pain that originates one place but is felt in another part of the body). So, three years after my diagnosis, and after my first hip scope, I was sent to a pain-management clinic for an injection into my SI in an attempt to isolate the origin of the pain. I brought my saddle and a stand so I could show them the position that was causing pain on my right side.
SI problems can cause lower back pain on one side or the other of the lumbar area. By doing a numbing injection into this joint, we were able to see that it had no correlation to the pain I was feeling when I swung my leg over the back of the saddle and my right seat bone made contact with the seat. I could not position my right leg without severe pain, even after this injection. Since the SI and lower back can be affected when one hip has a different range of motion than the other, the diagnostic team of health professionals can become confused between lower-back, SI and hip problems.
This next round of doctors’ appointments included a visit to my original surgeon as well as an out-of-state doctor who specializes in Birmingham Hip Resurfacing, a less-invasive treatment (hipresurfacingsite.com). The surgeon who had done my hip scope determined that the pincer portion (bony prominences on the rim of the hip) had not been sufficiently removed. However, there was still adequate space in the joint (meaning there was enough cartilage) to keep me out of the hip-replacement category. He suggested another arthroscopic procedure to smooth the rim, but there were no guarantees, and I was leery of doing the surgery.
The total hip replacement specialist I consulted was Dr. John Rogerson. He referred me to Dr. Christopher Larson, an FAIS specialist who concluded that my first hip surgery had been too conservative. Since the pincer portion hadn’t been removed adequately, it was still causing me pain when my leg went into certain positions. Larson uses a 3D CAT scan for diagnostic purposes. Having paid for my MRIs, X-rays and this scan out of pocket, I can assure you that this test was the best use of my money and everyone’s time and expertise. Larson felt the surgery would give me relief and was worth a try. I was willing to do another hip scope with him because during the procedure numerous X-rays would be taken with my leg in different positions to determine if the bony prominences were adequately removed. He wanted me to undergo another hip block just to be assured that the pain I was experiencing originated in the hip joint itself. I had a numbing injection in my hip joint when I returned to see my original surgeon that was not done correctly and clouded the picture for a while. This time, a hip block using X-ray guidance was prescribed.
My saddle, stand and I went in again to see the doctor who had performed the SI block. This test offered a positive result because I was pain free for about six hours. I rode as many of my horses as I could before the numbing meds wore off and I was back in pain.
Surgery was scheduled and immediately afterward I was able to feel the difference. As soon as I woke up, my physical therapist suggested I start my exercises. To my amazement, I was able to move my right leg into positions that had previously caused great pain. I flew home and began rehab again.
The first few months after surgery I was still on some restrictions, but I was bound and determined to do what I love most: ride dressage. My physical therapist, Rolfer and doctor allowed me to sign up for a clinic, as long as I didn’t overdo it, so off I went to clinic with Herbert Seiberl of the Spanish Riding School. Three months after my second surgery, I had the most magical lessons. Perhaps the new range of motion in my hip was the reason or maybe it was the weeks I spent imagining a ride like this.
I am still recovering financially and can’t buy the schoolmaster I had been saving for. I do not know how long either hip will last, but there is only slight pain on the surgical side when I ride and my other hip has some issues. For now, I simply enjoy being back in the saddle and I am grateful for the medical professionals who made that possible.
This article originally appeared in the July 2012 issue of Dressage Today magazine.