When your horse’s joints become stressed or diseased, you might hear your veterinarian talk about osteoarthritis (OA) or degenerative joint disease (DJD). Simply put, OA and DJD, in the natural progression of the disease process, are the degeneration of the cartilage and the synovial membrane, creating synovitis and bone remodeling. In the athletic horse, this degeneration of the cartilage is caused by reactive forces on the joint from the interaction of the horse’s conformation and the ground surface he is working on. It can also be caused by a traumatic wound incident involving the joint. But for our purposes, let’s focus on keeping joints healthy in the long run. Horses of any age can be affected by this issue, but you should be considerate of weight management, shoeing intervals and genetic predisposition.

The biggest factor in how the athletic horse is going to handle stress placed on his joints relies on a detailed conditioning program and correct riding. I find that horses who are conditioned to work on many different types of ground surfaces seem to have less joint trouble. Single-surface horses tend to have fairly predictable and specific injuries.
Horses are meant to move around constantly, not just for an hour each day. The more a horse walks in a day, the better. It’s the long, slow movements that will benefit your horse’s soft tissue and joint structures. If you are not getting 9s and 10s in your walk work, this is your opportunity to think about what you can do to improve the walk and help condition your horse’s joints, too. For example, when people see human physical therapists for injury, the work is slow, correct and deliberate. Your riding should be the same.
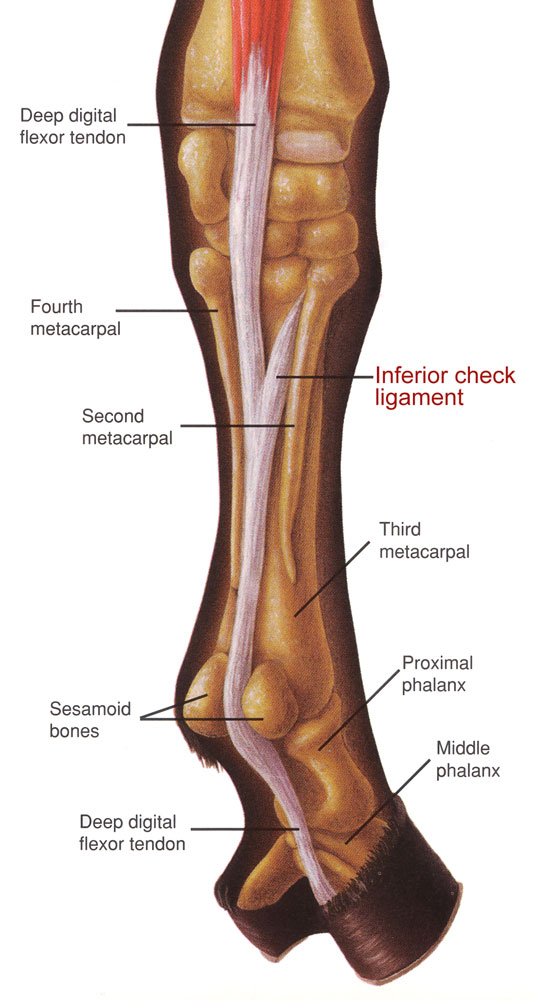
How does OA begin? Hard or deep footing, lack of traction, ligament strain, hyperextension or taking a bad step can contribute to the inflammatory cascade that produces synovitis. Clinically, we may observe a range of signs, from reluctance to perform, joint filling or puffiness (joint effusion) to overt lameness.
Basic preventive action begins with intimately knowing all the bumps and blemishes on your horse’s legs and noticing when one of them changes. For acute joint filling, icing is highly effective in 20-minute cycles up to several times a day. Support-bandaging after icing coupled with nonsteroidal anti-inflammatory drugs (NSAIDs) will keep a small problem from turning into a more chronic problem. Early detection does matter.
You can spend a lot of money on radiographs, ultrasounds, MRIs or CT scans, but most cases of OA can be diagnosed with a good static examination. This includes a thorough history of what has transpired, palpation and motion examination that leads to diagnostic analgesia, or blocking the joint with a numbing agent to confirm that the joint is actually contributing to the lameness. As the saying goes, we don’t ride radiographs. We ride horses who may have abnormalities on radiographs that do not cause issues. Joint blocks provide a high level of confidence in determining a specific diagnosis.
Unfortunately, there are no significant clinical signs that point to one joint. Any joint with dysfunction can cause similar clinical signs. If you are still wondering about a clicking sound within a joint, it comes from fluid movement/displacement within the joint and may not necessarily be a problem. Don’t forget that joints in the vertebral column can undergo primary joint degeneration and cause significant pain. I typically rule out and treat all limb lameness, then investigate the neck, back and pelvis when dealing with multiple joints.
Medical treatments start with NSAIDS as needed, such as phenylbutasone, flunixin meglumine (Banamine) or firocoxib (Equiox). All of these medications can cause ulcerations in the mouth, stomach or hindgut, and in my opinion, one is not better than the other. With your veterinarian as a guide, start with the recommended amount then try to reduce to the smallest amount that makes a difference. You should be concerned if it takes long-term daily NSAIDs to allow your horse to do his job. Be sure to talk to your veterinarian.
Joint injection with various combinations of steroids and hyaluronic acid is an effective treatment for effusive and painful joints that have been proven to be causing an issue by utilizing joint blocks. Regenerative therapies like stem cells, PRP and IRAP can work, too. We don’t know which treatment is best yet, but we are getting closer.
The main issue with supplements is that they are not controlled or regulated substances. A good way to know what you are getting is to use supplements that have been evaluated by the National Animal Supplement Council or a consumer lab. It’s the closest thing to having FDA approval. They evaluate claims and make sure the product contains what it promotes. They provide integrity and consistency in a very confusing market. You should also know that cost does not equate to efficacy. Just because you spend more doesn’t mean the supplement will do more.
Absorption of a supplement and its entry into the joint of the horse is the biggest question. There are a few ingredients we know that are absorbed orally and have been found to prevent and improve lameness using the racing Thoroughbred as a model. An oral glycosaminoglycan called hyaluronic acid is one of them. The studies on avocado’s, soy’s and omega 3’s effect on inflammation are also very promising.
Intramuscular injectables, such as Adequan and Pentosan, are for cartilage repair and maintenance. The labeled dose is every four days for a series of injections. Many horses receive injections in a much longer interval and, therefore, may not be getting the full benefit the owner believes they are providing. Legend is a mid-range molecular-weight hyaluronic acid. Truthfully, we are not sure how it really works as it does not have a long-term effect (2 to 4 days) but it is very effective when there is an acute synovitis. I tend to believe that if Legend is working, oral hyaluronic acid will work, too, and not require the injections.
A new trend is administering intravenous biphosphonates, such as Tildren or Osphos. They are useful for bone edema or when osteoarthritis is advanced. They provide bone-pain relief by inhibiting osteoclasts. It can be a very effective treatment when used appropriately.
For the long haul, while you are moving through the levels with your horse, keep a detailed calendar of how your horse is doing, what his exercise level is and the response to different treatments that you have tried. The basic fundamentals of horsemanship and ice will go a long way in the prevention of osteoarthritis.