Q: I have an 11-year-old Morgan gelding who has successfully competed through Prix St. Georges with no joint injections. But he is now struggling with Intermediaire I. Oral supplements and managed shoeing practices are no longer helpful by themselves. I would like to now consider joint injections, but the one issue holding me back is the corticosteroid being used. How is the dosage different from the anabolic dosages used in the past? My concern is maintaining the integrity of the joints long term. Does the currently used dosage cause long-term damage?
A: These days veterinarians have a myriad of products to choose from for intra-articular injection therapy. When selecting a product, considerations include age of the horse, previous response to intra-articular therapy, whether or not there is pre-existing disease in the joint and, finally, concurrent disease in the animal as a whole (e.g., Cushings disease).
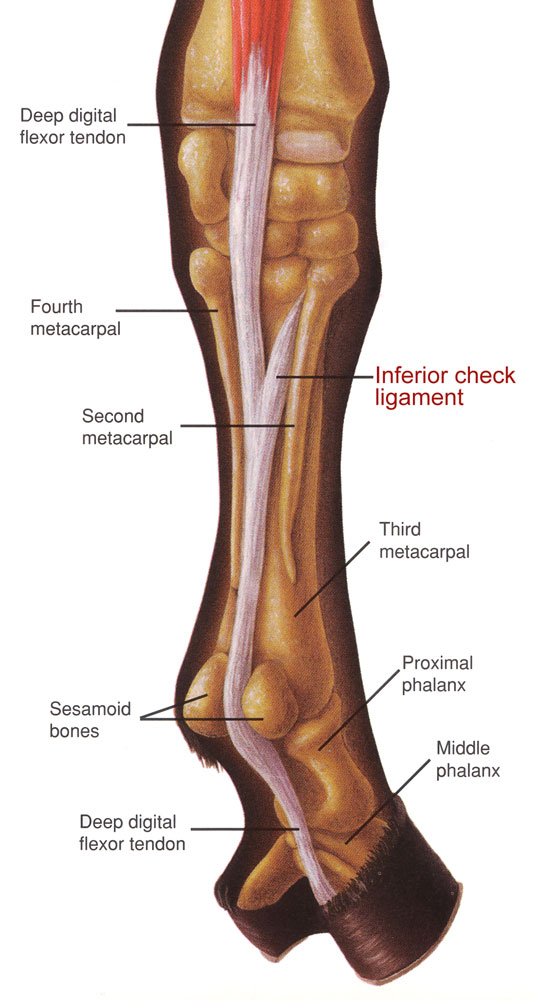
therapy delivers
powerful relief
where a horse
needs it most. (Photo by Amy K. Dragoo)
There are two basic broad categories for consideration: steroids or regenerative products. The word “steroid” can be intimidating, and owners should understand that veterinarians are not recommending the products that we hear abuse scandals about, which are in the category of anabolic-androgenic steroids. Rather, equine sports medicine utilizes a subset of steroids called corticosteroids, which have powerful anti-inflammatory properties. Most horse owners are familiar with a basic medication in this category, dexamethasone, which is commonly administered orally to horses for systemic inflammatory conditions like hives or a cough. More refined versions of corticosteroids are utilized routinely for targeted joint injections. Studies have evaluated their efficacy and safety, and when used judiciously these medications do not have long-term negative effects on the health of the joint.
My typical corticosteroid choices for joint injections include triamcinolone and betamethasone, and I inject them into joints in combination with hyaluronic acid. Hyaluronic acid is a component of healthy joint fluid and provides the lubrication between the cartilage surfaces to help them move comfortably. In joint inflammation, the level of hyaluronic acid is reduced so injecting it into the joint helps to immediately restore the normal viscosity and homeostasis within the joint. The anti-inflammatory benefits of this style of therapy have a quick onset and in many cases a horse can return to exercise in four to five days. This short downtime is an advantage in horses who are in full work or training for an upcoming competition. Both this short break from training and drug withdrawal times need to be considered when planning injection therapy in close proximity to U.S. Equestrian Federation or FEI-regulated shows.
In some cases though, we need an alternative to corticosteroids. Regenerative medicine is a big topic of discussion in both animals and people. It offers a way to manage inflammation without deleterious effects on the local environment or whole patient, and even the potential to heal injuries that previously have not responded to therapy.
For horses, the choices you may have heard about include interleukin-1 receptor antagonist protein (IRAP), platelet rich plasma (PRP) or stem cells. A scenario that might push a veterinarian to consider one of these is an older pony with a history of laminitis. Since corticosteroids are very similar to the endogenous steroid hormone cortisol, which can become uncontrolled in equine cushings disease, injecting more corticosteroid into such a patient can trigger swings in insulin and glucose and exacerbate the clinical signs of diseases like cushings or equine metabolic syndrome. For these patients, a veterinarian may prefer switching to an anti-inflammatory product that is created from the horse’s own blood and doesn’t have systemic ramifications.
Another indication for a regenerative product is when there is an injury within a joint, for example to the cartilage or subchondral bone, or an injury to an adjacent soft tissue and the local effects of the steroid could affect healing. While corticosteroid injections don’t necessarily shorten the lifespan of a joint, degenerative joint disease can happen over a horse’s lifetime and in some cases injection therapy with corticosteroids is no longer sufficient to control the inflammation.
Regenerative products offer a way to extend the athletic career of horses in a safe way as well as the potential to recover from injuries that previously carried a much more guarded prognosis. There are disadvantages to regenerative products, namely the significantly higher cost when compared to traditional joint injections. Another factor can be availability, both in your local marketplace and for your horse at the time you determine the need. The good news is that as this field achieves advances and the scientific literature provides further evidence of efficacy, regenerative therapies are becoming more accessible. Biotech companies continue to refine harvesting techniques and develop options that can be applied in the field.
Whichever choice is made for your horse, the goal is the same: to decrease the inflammation within the joint and keep your horse comfortable enough to do his job. This strategy can ultimately extend the athletic lifespan of a horse by mitigating the downstream effects of persistent inflammation, which leads to joint degeneration. As you mentioned, systemic medications and joint supplements certainly have their place, but targeted joint therapy delivers powerful relief where a horse needs it most.
This column has not been approved or endorsed by U.S. Equestrian.
Christina “Cricket” Russillo, DVM, graduated from the Tufts University School of Veterinary Medicine in 2001. After completing a large animal medicine and surgery internship at Texas A&M, she realized her desire was to work on elite sporthorses. Following 13 years of practice at Fairfield Equine Associates in Newtown, Connecticut, focused on high-level show-jumping and dressage horses, she joined Virginia Equine Imaging in 2015. Russillo relocates to Florida every winter to support her clients and patients. She has competed through Third Level in dressage, and in February 2017 she was appointed the U.S. Dressage Team veterinarian.