We’ve all seen those hunter/jumpers who really “snap” their knees over fences. And how about those dressage horses whose extravagant knee action prompts a collective gasp from spectators? Good or bad, function or fad, a sporthorse’s athleticism is defined in some measure by how these joints perform. As they bend, extend and compress—supporting considerable weight and enduring repeated concussion—strong, flexible knees help ensure a clean jump, a ground-covering stride and eye-catching movement—until they don’t.

© Amy K. Dragoo
Trauma to the knee can occur in a number of ways in any type of horse and at any age. Faulty conformation can be a factor, with offset joints (“bench” knees) or outside, forward or backward deviations carrying an increased risk of injury and lameness. However, regardless of build, the more a sporthorse is campaigned, the more likely he is to incur wear and tear or outright injury to this complex, weight-bearing joint.
Early diagnosis of the nature of the problem, followed by timely, conscientious treatment, offers the best chance of keeping an acute knee injury from turning chronic and possibly ending a sporthorse’s career.
Diagram of an Equine Knee Injury

First, a very basic anatomy lesson about a joint that is anything but basic:
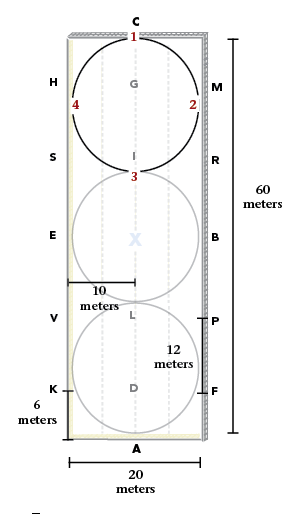
The horse’s carpus, or knee, consists of a number of small bones that form two rows and connect in three primary sub-structures: the radiocarpal, intercarpal and carpometacarpal joints (see diagram on right). Most of a horse’s weight is carried in the medial aspects (the inner half) of the radiocarpal and intercarpal joints, with movement occurring on the medial side of the knee.
These bones, which join the radius at the top of the knee and the cannon and splint bones below the knee, are held together by a complex series of ligaments. Besides maintaining joint stability, these ligaments act as shock absorbers during motion. The knee problems most common in sporthorses generally fall into one or more of the following categories, keeping in mind that they sometimes overlap. In laymen’s terms, these are:
1. Soft tissue injuries (the ligaments, cartilage, etc.) in and around the joint. This is what generally occurs in twist sprains, strains, pulls, etc., and can include a common condition called proximal suspensory ligament
desmitis. A “big” or “popped” (swollen) knee can be indicative of merely tissue inflammation, or the inflammation could be part of a more complex situation involving the structure beneath it.
2. Wounds. Gashes, lacerations and the like can be either superficial or extend deeper into the tissue. Like the inflammation that often accompanies them, they can also be just one component of a more complex injury involving the knee’s inner workings. Loss of synovial fluid (the joint’s essential lubricant), the potential for infection of the joint (which can become chronic) and scar tissue buildup can be complicating factors in this type of knee injury.
3. Bone issues. Trauma and wear to the joint, as well as accompanying inflammation, can result in regenerative changes to the bone (such as
remodeling or increased density—think bone spurs), not to mention chips and fractures. Included in this category are ailments like subchondral bone disease of the third carpal bone and third carpal bone sclerosis (or even both), which are seen a lot in racehorses.
4. Osteoarthritis. Just like in humans, this degenerative disease develops in joints as a result of trauma or just plain wear and tear; inflammation is both a contributing factor and a result. In equines, one type of osteoarthritis develops as a response to stress-related changes, fractures or chips in the bone and damage to the cartilage (think young racehorses in hard training, for example). A second type, seen more often in older horses, appears to develop without the same cycle of exercise-induced bone and cartilage remodeling and damage. Over time, loss of synovial fluid results in a gradual decrease/breakdown of cartilage thickness and an increase in friction within the joint (bone rubbing against bone). This degeneration, combined with weakening of related ligaments, can produce the “creakiness” and instability often associated with arthritis in a senior equine. Like your grandpa’s “trick knee,” this is often what is occurring in a “chronic” knee problem.
Diagnosis
It’s hardly surprising that acute knee injuries are most common in disciplines involving speed and/or jumping. They are often the immediate result of trauma and will occasionally require surgery.
By contrast, “wear and tear” to the joint can occur over time in virtually any horse sport, simply as a result of repetitive motion; this can present as either a gradual, intermittent or sudden-onset lameness. “One acute overuse soft-tissue injury in the back of carpus is proximal superficial digital tendonitis, aka ‘high bowed tendon,’” noted Elizabeth J. Davidson, DVM, DACVS, DACVSMR, associate professor of Equine Sports Medicine at New Bolton Center in Kennett Square, Pennsylvania. “This injury most commonly occurs in the middle-aged or older sporthorses,” she added.

© Amy K. Dragoo
Regardless of the cause, one thing is clear: Early intervention is critical if treatment and rehabilitation of an acute knee injury are to be successful.
“In the sporthorses I see, the most common knee injuries are typically from hitting their knees (on something such as a jump), falling on flexed knees or sustaining lacerations,” noted Caitlyn Horne, DVM, ACVSMR Equine Sports Medicine and Rehabilitation at North Carolina State University’s College of Veterinary Medicine. “Getting an early accurate diagnosis of what structures are involved—and to what degree—helps [us] make early, more effective treatment decisions. Treating a knee once the process of osteoarthritis has already started or a significant scar has already formed is going to be more difficult.”
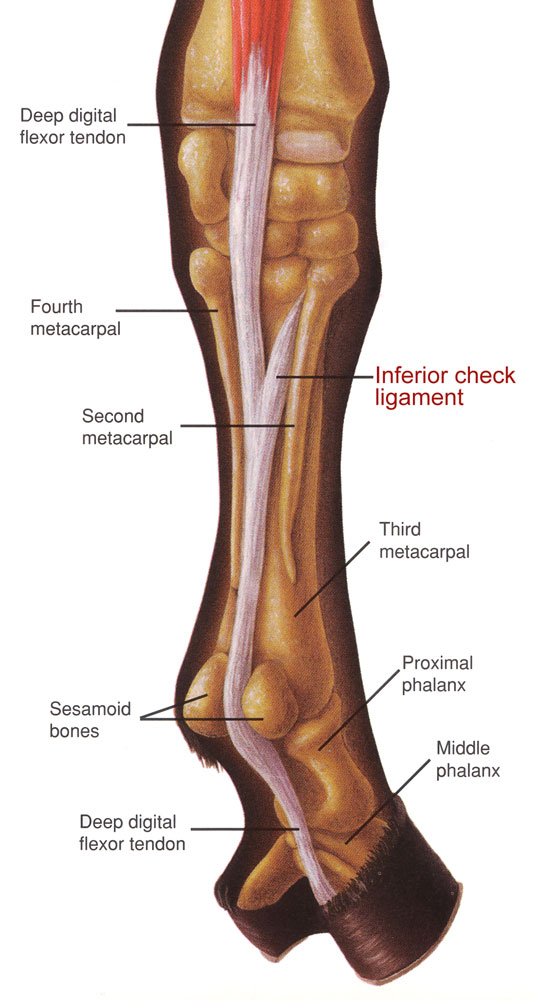
Dr. Davidson stressed the same point, adding, “The knee is a complex anatomical structure. There are many small carpal bones. There are important soft tissue structures along the palmar (back) of the carpus.” This includes the aspect of the suspensory ligament that lies just below and behind the carpus.
“There are also important synovial structures including the carpal joints, joint capsules and the carpal canal. Acute knee injury can damage any of these anatomical structures depending on the type of injury. Also, the dorsal carpus has extensor tendons and tendon sheaths.”
Unless the injury’s location is painfully obvious, a lameness is generally traced to the knee through a combination of physical examination, gait check, flexion tests and nerve blocks.
Then the real work begins; because the knee involves so many parts, X-rays and ultrasound are especially useful in pinpointing the exact nature of the problem. “In acute injury, the carpus may be swollen, which can make acute identification of underlying internal damage to the important bone and/or soft tissue structures of the carpus difficult,” Dr. Davidson said. In these cases, advanced imaging like magnetic resonance imaging (MRI) and computerized tomography (CT) scans might be necessary to determine which structures are involved. By contrast, swelling can be subtle or even absent in some knee injuries, Dr. Davidson noted, “ … especially palmar [back] of the carpus injuries. Veterinary evaluation including diagnostics is recommended.”
Wounds and/or lacerations to the knee present yet another set of potential issues. “It is important to assess if the wound communicates with a synovial structure and/or has caused penetrating damage to the bones and/or soft tissues,” Dr. Davidson said. “Without prompt identification, a wound that penetrates a synovial structure can result in an infected joint or tendon sheath,” she added, noting that “chronic sepsis of a synovial structure is very difficult to treat effectively.”
After applying cold therapy to a knee injury to reduce inflammation and swelling, the knee might be bandaged initially to immobilize it and to prevent infection if the injury involved a wound or laceration.

© Amy K. Dragoo
Treatment
The type and length of treatment that is required to heal a horse’s “bum” knee will naturally depend on the type, location and degree of the injury. Considerations to determine these factors include which tissues are involved, whether the joint or carpal sheaths are implicated, whether there is a wound, cartilage tears or damage to the bone, etc.
If a ligament has been torn, for example, prepare for weeks or even months of rest, hand-walking and a gradual return to exercise as dictated by your veterinarian. As Dr. Davidson noted, “Soft tissue injuries tend to take longer to heal and often required prolonged confinement and controlled exercise program. If the soft tissue injury is missed (not identified), the horse may inadvertently be placed back into exercise too quickly; the missed soft tissue injury may not have healed adequately which may prolong healing and/or result in re-injury.
“Bone fragmentation and/or small fractures can also be missed without veterinary evaluation, and without adequate and appropriate treatment, any joint injury can result in
arthritis,” she said.
Generally speaking, the first priority after a knee injury will be decreasing any heat and inflammation. This is important to help reduce both the pain now and the risk of chronic degeneration (and even more pain) down the line.
Conventional anti-inflammatory treatment usually starts with cold therapy, such as icing or poultices, immediately after a traumatic injury. The knee might also be bandaged initially to immobilize it. Then, depending upon the diagnosis, non-steroidal anti-inflammatories such as phenylbutazone (bute) might be given to address the pain, keeping in mind that the risk of gastrointestinal and kidney issues increases with long-term use of NSAIDs. Going forward, your veterinarian might consider regular use of anti-inflammatory medications or even injections of drugs (either non-steroidal or steroidal) to address chronic knee problems.

© Amy K. Dragoo
Corticosteroids can provide powerful, even dramatic relief of inflammation and pain. Some types also offer a degree of joint protection and—if administered with hyaluronic acid—joint lubrication, as well. However, it’s wise to reserve corticosteroids in particular for conservative use when nothing else seems to work. This is because excessive or long-term administration of certain steroids can, ironically, result in cartilage breakdown and even contribute to the onset of laminitis.
Polysulfated glycosaminoglycan (Adequan®) or hyaluronate sodium (Legend®) injections are common non-steroidal options for maintaining joint soundness in older sporthorses. Adequan is said to help increase HA production and decrease synovial inflammation, while Legend is reportedly intended to treat joint dysfunction related to synovitis (inflammation of the synovial membrane) associated with osteoarthritis.
And don’t discount novel regenerative therapies; these are gaining popularity as alternative ways to treat joint issues without steroids. “The regenerative therapy that we use most commonly in the knee is IRAP [Interleukin-I Receptor Antagonist Protein],” said Dr. Horne. “We use this in multiple ways, as an anti-inflammatory after an acute injury, as a post-operative series after surgery or as a maintenance therapy for a chronic knee injury.”
For older horses who have sustained knee injuries, a “whole-body” approach might also be worth exploring because over time, an injury in one leg can lead to overcompensation and soreness elsewhere, too. Possible treatments along these lines include judicious non-steroidal therapy in the form of either phenylbutazone or firocoxib, a COX-2 inhibitor that can often be given to
horses who are sensitive to more conventional NSAIDs.
Rehab Best Practices
The length of confinement and rehabilitation required by a knee issue—and the timing of a controlled exercise program—will obviously vary with the diagnosis and severity of the problem(s).
Of particular concern during rehabilitation is maintaining the complex range of motion in such a normally flexible joint. “One of the common issues I see in treating and rehabbing acute and chronic knee injuries is that flexion of the knee can be very painful,” Dr. Horne commented. “It is important to address this early, as it can then turn into a chronic problem that is more difficult to treat.
“The knee is normally capable of a large degree of flexion, and it is important after any type of injury to keep this range of motion,” she explained. “In the acute stage, it is important to try to get the horse as comfortable as possible quickly by decreasing the associated swelling and any intra-articular effusion [fluid accumulation within the joint]. Sometimes this can be done with just simple things, such as cryotherapy [icing] and compression bandaging.
“Once the horse is comfortable, initiating early range-of-motion exercises is critical in order to prevent future loss of range of motion and encourage a healthy joint environment,” Dr. Horne continued. Depending on the case and comfort level, she said one could start with just passive range-of-motion exercises (ask your vet to demonstrate) or both passive and active range-of-motion exercises, such as work over ground poles and cavalletti.
Range-of-motion exercises can be tricky, however, where wounds and lacerations are concerned because of the risk of tearing the wound open. Wounds also bring with them the prospect of scar tissue buildup, which can further impede motion over time. “We do see chronic scars from old wounds or extensor tendon injuries [over the knee],” Dr. Horne confirmed.
Because of this, she said it might be necessary in such cases to temporarily limit knee motion to allow the wound to heal more effectively. This is why “… getting early veterinary care can be very important in these cases,” she said, adding, “Once the wound has healed, addressing the scar early is important to prevent decreased range of motion later.”

© Amy K. Dragoo
So, let’s say your horse got lucky—he wrenched his knee but appears to have recovered; the swelling has subsided, and he now seems to be moving sounder than ever. However, if he didn’t have a full veterinary evaluation, don’t be fooled by appearances, Dr. Davidson warned.
“Many horses become comfortable and/or sound BEFORE the underlying injury(s) has healed, which can give one a ‘false sense’ of security about the actual tissue healing,” she said. “And a too-early return to exercise and/or turn-out can result in re-injury of an inadequately healed injury. Therefore, relying on the horse’s comfort as the only criteria to determine if the horse is ready to go back to work can be inadequate and misleading,” she explained.
To this end, Dr. Davidson recommended periodic re-assessment of both horse comfort and the actual injury by a qualified veterinarian. (Ultrasound scans are one tool that can be helpful here.) “Minor injury might require a few re-assessments. Major injury might require numerous periodic re-assessments throughout the injured tissue’s healing process,” she noted.
Conscientious conditioning and management will go a long way toward maintaining a rehabbed knee and even preventing future knee injuries. Four key takeaways:
- During your horse’s “down time,” do as much as you can—within comfortable levels—to maintain his knee’s range of motion.
- Whether bringing your horse back from injury or maintaining his usual schedule, make any changes in the type or intensity of his work gradual. Space out longer sessions and keep a close eye on his responses.
- Bear in mind that the fibers in torn or stressed ligaments heal/remodel slowly, and the “repairs” might be weaker, less elastic and more prone to injury than before.
- Remember that every case is different, and knees, like all joints, undergo changes over time. Keep your veterinarian apprised of your horse’s progress and seek his or her guidance about how to proceed.
A word here about oral supplements: Formulas with glucosamine and chondroitin sulfate in particular are widely used these days to support equine joint health. Experts generally view oral supplements as less effective than injections at reducing pain, inflammation and discomfort after a joint injury. Where some theorize oral supplements might be most helpful is in the prevention of osteoarthritis in joints that have not yet sustained trauma.
This last part is important since, as Dr. Horne noted, “Osteoarthritis is probably the most common chronic knee problem that we see.” She went on to say, however, “I do not think chronic joint problems are necessarily inevitable, as there are lot of factors that play into osteoarthritis, such as genetics, the job of the horse and how the horse has been managed.
“I think we continue to learn a lot about joint health and have learned a lot from human medicine about [the fact that] early rehabilitation intervention is critical to help reestablish a healthy joint environment.”
This article originally appeared in the Spring 2022 issue of Practical Horseman.